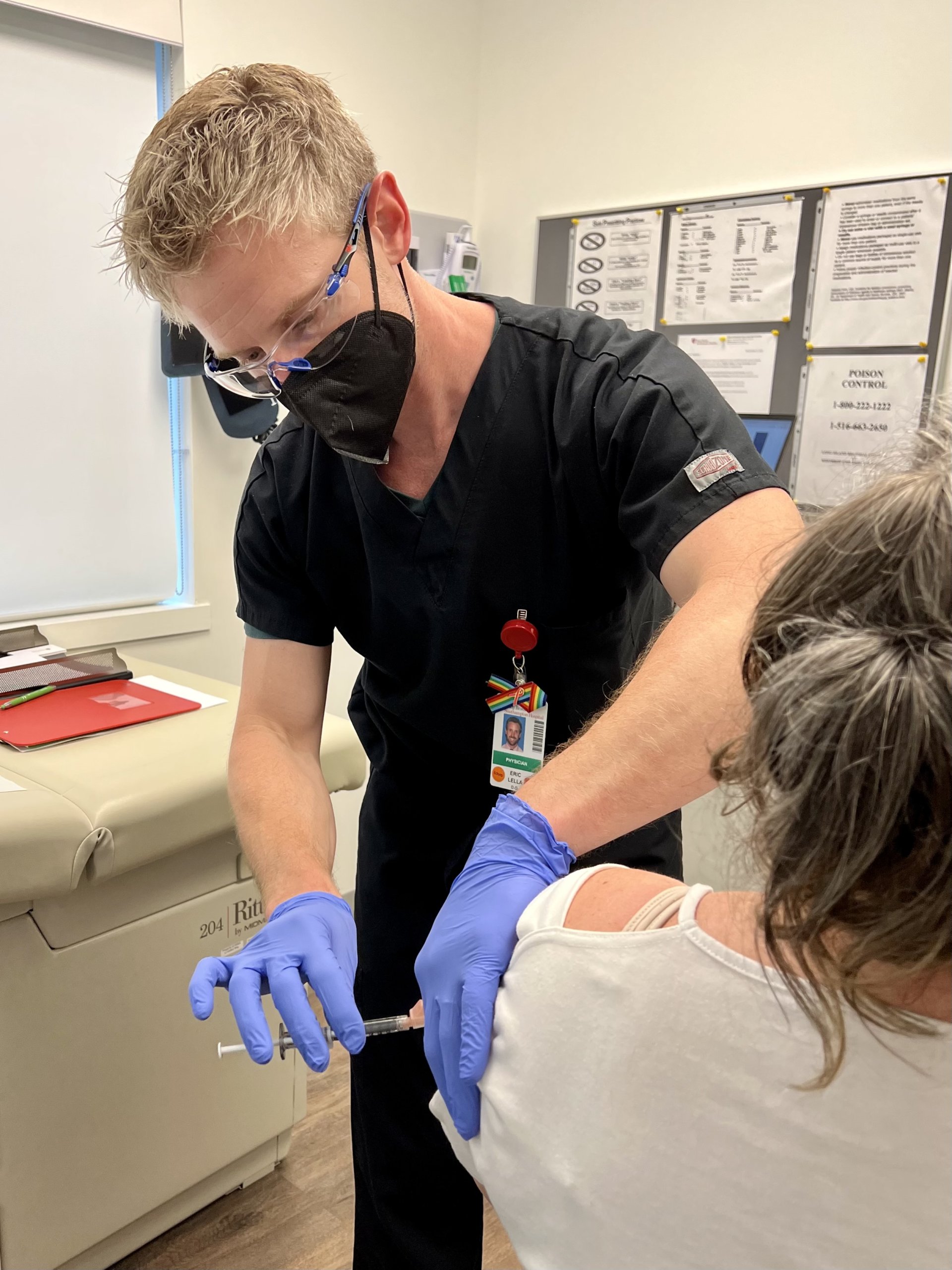
Dr. Eric Lella Talks Monkeypox, Vaccines, New HIV Care Advancements & More at the Edie Windsor Healthcare Center

First COVID, now monkeypox. It’s been another year of alarming health headlines.
With the United States in the midst of its largest-ever monkeypox outbreak (New York City is the epicenter of the current outbreak, accounting for more than 25% of the cases in the U.S.; there are currently four confirmed cases in Suffolk and one in Nassau, according to the CDC), we thought it was a good time for a wellness check-in with Dr. Eric Lella, the Director of the Edie Windsor Healthcare Center in Hampton Bays which just this week administered 250 doses of monkeypox vaccines that it received from the Suffolk County Department of Health.
Dr. Lella shared his insight on monkeypox and its risk to the LGBTQ+ community. He also discusses the latest in HIV care and prevention and the importance of primary care and routine screenings for overall wellness and good health.
A Chat with Dr. Eric Lella on Monkeypox, HIV Care & More
Before we get to monkeypox and the new pop-up vaccine clinic, outline the services you provide at the Edie Windsor Healthcare Center.
We provide HIV treatment, HIV prevention, comprehensive STI (Sexually Transmitted Infections) screening (the medical community calls it STI, we don’t call it STDs anymore), mental health services for HIV and LGBTQ+, primary care/family medicine — includes: adolescents, teenagers, adults, geriatrics, women’s health (pap smears, DEXA and mammogram ordering).
There’s no stigma here. I tell my patients, “I’m a gay man, I’ve heard it all, I’ve got plenty of LGBT friends — nothing is going to shock me.” This is a comfortable space, we talk freely, we don’t have to be fearful. The main reason for coming here is the patient can feel comfortable because we’re already aware of all these different types of sexual practices that we know we need to screen for.
Tell us about the new monkeypox pop-up clinic out east.
The monkeypox pop-up vaccination clinic at the Edie Windsor Healthcare Center (Hampton Bays) opened this week (two days: July 18 and July 22). Appointments filled up within 48 hours for the limited doses of the monkeypox vaccine (500 doses, enough for 250 people) that we received from the Suffolk County Health Department. We heard about scheduling sites for other vaccination pods that crashed within the first 30 minutes after the announcement. It’s bonkers in the city.
Out east, more doses will be available in the future and we encourage people to constantly check the Suffolk County DOH Monkeypox resources site at suffolkcountyny.gov/monkeypox for the most current updates. Dates will be added as they become available.
What is monkeypox and why is it of particular concern to the LGBTQ+ community?
Monkeypox is a virus in the same family as smallpox, cowpox, horsepox, camelpox, but with slightly different symptoms. It had surfaced mainly through humans and animals in Africa and is spreading internationally. It is a rare viral infection that can cause rashes, bumps, or blisters on or around the genitals or in other areas: hands, feet, chest, or face, that may be itchy or painful. It can also cause swollen lymph nodes, flu-like symptoms, such as fever, headache, muscle aches, chills, and fatigue. These symptoms may occur before or after the rash appears, or not at all.
The monkeypox case-fatality ratio in recent times for the West African clade of monkeypox has been 1% and might be higher in immunocompromised persons, according to the CDC. Monkeypox is usually a self-limited disease with symptoms lasting from two to four weeks.
Anyone can contract monkeypox, but those with a higher risk of exposure to monkeypox include members of the gay, bisexual, transgender, and gender non-conforming community, and other communities of men who have sex with men and who have engaged in intimate or skin-to-skin contact with others in the past 14 days in areas where monkeypox is spreading.
How is monkeypox spreading?
Monkeypox is spreading in large communal gatherings and certain sites — clubs, sex parties, bars — where lots of people are crowding into small spaces and there’s prolonged skin-t0-skin contact and exposure to respiratory secretions — so if a lot of people are at a circuit party and they are all shirtless and they are all breathing on each other, that’s two forms of possible transmission.
The common use of dating and hookup apps has been a contributor to the fast spread in this community.
Monkeypox can also spread through shared towels, clothing or sheets, so if somebody with monkeypox is sleeping in bed sheets and somebody else sleeps in those bed sheets, they can potentially spread it.
There are reports of many shortages and delays in getting monkeypox vaccines — why?
The current monkeypox vaccine has been around and was FDA-approved in 2019 (it covers for smallpox as well). They are manufactured in Europe by a small company, we are just waiting for additional FDA approval from the production sites and for it to be released from storage and then sent to state and county health departments who release it to community vaccination sites.
It is all frozen and has to be handled properly, it can’t just be FedEx-ed overnight to the clinics. The monkeypox vaccine is two shots, given four weeks apart.
Switching gears, what are some of the newest treatments for HIV?
The older regimens used to be multiple pills and sometimes multiple times a day. We have some newer treatments that can potentially take it down to a single pill daily for some patients.
The newest HIV treatment available over the last couple of months is an injectable medication which we do here in the office that is every two months; the patient is given an injection and that is their HIV medication, they do not have to take a daily pill and that keeps them virally suppressed. Its brand name is Cabenuva.
There are some injectable medications that are in trials right now that would potentially bring that out to an injection every six months.
Explain PrEP in terms of HIV prevention.
PrEP (Pre-exposure Prophylaxis) is a medication that will prevent those at risk from contracting HIV.
PrEP for HIV prevention was first approved by the FDA in 2012 and finally there has been a larger campaign for it to be offered more widely to anybody who is at a higher risk — that includes men who have sex with men, sexually minoritized women, transgender individuals, IV drug users, anybody who has multiple sexual partners or anonymous sexual partners that they are not using protection with, and that extends out to people who are having anonymous sex and while using party drugs.
That’s where the risk of infection can be quite high because that’s when condom usage kind of goes out the window.
PrEP, if taken daily without missed doses, is over 99% effective. It is covered by insurance and a couple of years ago the federal government upgraded it to a Category A recommendation meaning that all insurance companies have to cover it. (Brand names are Truvada, Descovy.)
Most exciting, there is also a new injectable form of PrEP that just came out — the brand name is Apretude — that’s an injection in the office every two months and no daily pill is needed.
How has HIV care improved over time?
If somebody is adequately treated and we achieve a viral suppression, undetectable equals untransmissable and that’s one of the important parts of HIV care. It’s not a death sentence if caught and treated properly.
The goal is to screen for HIV often and link any newly diagnosed patients to immediate care. If we can get patients on medication regimens and virally suppressed, they’re going to have a normal life span.
What specific primary care do you recommend for the LGBTQ+ population?
Many LGBTQ+ patients will skip screenings because they either don’t feel they are at risk or they lack access to primary care. Studies show the LGBTQ+ community has higher rates of substance/alcohol/tobacco abuse, obesity, risk of physical and sexual abuse/intimate partner violence.
We recommend regular health maintenance screenings: colon, breast, cervical, anal cancer screening. We offer comprehensive STI screenings specific to all types of sexual practices that isn’t typically offered at other primary care offices.
Different sexual practices carry different risk factors so proper immunizations are important.
We also need to think about proper mental health screenings. We know that mental health illnesses are much more prevalent in the LGBTQ+ community than they are in the general population, so we need proper LGBTQ+ affirming psychiatry care and therapy services.
We are continuing to expand our mental health services for the LGBTQ+ community and for our primary care patients, both LGBTQ+ and non-LGBTQ+.
The Edie Windsor Healthcare Center (EWHCC) providing LGBTQ+ Healthcare and HIV/AIDS Care and Prevention Services, via Rose Walton Care Services, is located at 182 W. Montauk Highway, Building B, Suite D, Hampton Bays. Office hours are Monday–Friday, 8 a.m.–4 p.m. Bilingual English and Spanish language staff. For monkeypox vaccine updates and availability, visit suffolkcountyny.gov/monkeypox.
Scheduling future monkey pox vaccines at EWHC will only be available online.
For eligibility requirements and more, visit southampton.stonybrookmedicine.edu/services/LGBTQ-and-HIV-healthcare.



