Why Women's Heart Health Deserves Our Attention on Wear Red Day

The nation is putting a spotlight on women’s heart health by wearing red this Friday, February 3. It’s no coincidence that February is also American Heart Month, which may lead some to ask, why are we putting the spotlight specifically on women when so many more men die of heart attacks and heart disease?
Dr. O. Wayne Isom, an East Hampton resident and world-renowned heart surgeon — yes, the one who famously turned down former President Bill Clinton for surgery in 2004, supposedly to play golf in the Hamptons (though that’s not quite the true story) — offers some insight into the facts about, and the unique complexities and difficulties involved with, women’s hearth health and disease.
First, it should be noted that the Centers for Disease Control and Prevention says heart disease is the leading cause of death for women in the United States. In 2020, the CDC reports that 314,186 women died, which was about 1 in every 5 female deaths, while 382,776 men, or 1 in 4, died of heart disease.
That said, numerous reports also note that a woman is more likely to die of a heart attack than a man.
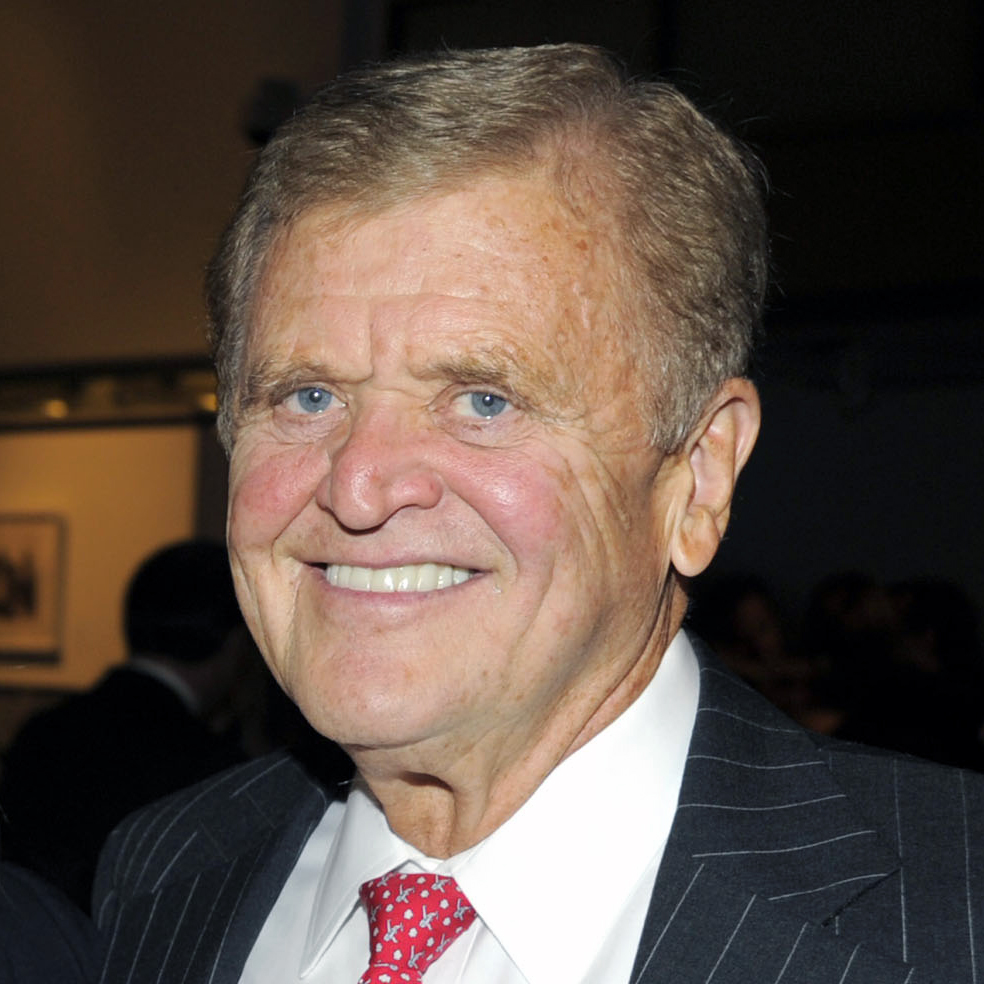
Dr. O. Wayne Isom on Women’s Heart Health
“The invasive treatments such as coronary bypass or stents, the mortality is higher in women than in men,” Dr. Isom says, explaining why women’s heart health is so important.
Symptoms are often more difficult to recognize in women, which can lead to delays in diagnosis and, ultimately, treatment — and delays in treatment can result in deaths.
“Women have atypical pain, they have atypical symptoms,” Dr. Isom points out. In fact, 40% of women who have heart attacks have no chest pains. “A man with coronary disease many times will have what’s known as crushing substernal chest pain. It may radiate out into the heart, but women classically don’t have that.”
He explains that women may have a hard time describing their pain since it’s not the classic “squeezing” chest pain or pressure, or pain or numbness in the left arm or shoulder. “They may have pain in the right shoulder,” Dr. Isom adds, recalling his work treating the wife of an orthopedic surgeon who suffered from pain in her right shoulder when she played tennis.
“The orthopedic surgeon, her husband, had injected the shoulder for bursitis several times to no avail. She ultimately had a cardiac catheterization (inserting a catheter into a chamber or vessel of the heart for diagnostic reasons) and it revealed coronary disease. I operated on her and her shoulder pain disappeared. That’s an example of how women have atypical pain,” Dr. Isom says.
“If you read in the textbooks, heart pain does not manifest itself in the right shoulder, it’s mainly in the left shoulder. But doctors in general many times don’t recognize women’s pain, so they may be treated later than men because it’s not picked up.”
And that’s not the only complication with women’s heart disease.
According to a 2015 lecture by Dr. Isom and his colleague Dr. Holly Andersen, 36% of women do not call 911 when they are having a heart attack, women’s hearts are smaller and beat faster making it harder to diagnose, women are more sensitive to drugs and, in general, a woman is less likely to be diagnosed than a man.
“One of the other reasons is women have smaller vessels, and the coronary vessels are (already) very small,” Dr. Isom says, noting women’s coronary vessels are usually around 1.5–2 millimeters — or, as he describes it, “about the size of a pencil lead.”
“If you’re doing surgery and you’re operating on something the size of a pencil lead, it’s really, really small, so the technical expertise is really trying. You have to have magnification of small vessels and small needles just to technically do a good job,” he continues.
This can be problematic with stents and/or angioplasty (two ways of opening narrowed or blocked arteries) because it’s much easier to injure a small vessel, or for the tiny stents to clot, causing a potentially deadly blockage called stent thrombosis.
“Men in general are bigger than women, and that’s not just their hands and their height and their feet, that’s the vessels in their heart, too. That’s something that’s not recognized,” Dr. Isom says.
It’s best to avoid heart disease in the first place, obviously, but this is especially true for women’s heart health and women’s heart disease which is harder to treat and diagnose.
But there are plenty of ways to significantly reduce one’s risk for heart disease, according to Dr. Isom, who shares some simple choices that can make a difference to women (and men) trying to stay healthy.
First and foremost, stop smoking. It is, of course, a major risk factor for heart disease and many other illnesses.
“Keep it very simple. You can make your life miserable by worrying about what you eat, whether it’s a man or a woman,” he says. “You stay away from real fatty foods. Eat a number of vegetables. Try not to get overweight. Fruits and vegetables are important. And try to get on an exercise program.”

Dr. Isom points to a Mediterranean diet — which has been said to reduce all causes of mortality — as resulting in a 30% decrease in death from stroke and heart attack. He also suggests avoiding refined sugar, which make people hungry and eat more.
“As far as exercise, you don’t have to get out and jog 5 miles a day. You can just walk briskly, like for 20 minutes a day, five days a week. That will also help you,” he says.
He also explains that women (and men) should regularly check their blood pressure, as high blood pressure can result in atherosclerosis, or a narrowing of the arteries.
“Many times, there’s somebody who goes along and they look healthy, they act healthy and they’ve got high blood pressure and never even knew it, until they go to the doctor and get a check. So you should know your blood pressure,” Dr. Isom says, adding, “Somewhere along the line, after (age) 25 or 30, somewhere in there, you should have your cholesterol checked, too.”
High cholesterol also causes atherosclerosis and it can be managed by improved diet and/or medications such as Lipitor, which lowers cholesterol in the blood.
Finally, Dr, Isom acknowledges the value of being your own advocate when it comes to women’s heart health. “Doctors aren’t perfect,” he says. If you are having symptoms after one doctor says nothing is wrong, “Go to another doctor and get another opinion,” he says.
Learn more about women’s heart health and Wear Red Day at goredforwomen.org.
Dr. O. Wayne Isom has operated on celebrities such such as Walter Cronkite, David Letterman, Regis Philbin and others — but not Bill Clinton (he was never told who he was turning down). He is retired from surgery, but still consults with select patients and remains a Professor of Cardiothoracic Surgery at New York Presbyterian-Weill Cornell Medical Center in NYC, where he was chairman of Cardiothoracic Surgery for 30 years. Dr. Isom is also on the board at East Hampton Healthcare Foundation and Stony Brook Southampton Hospital.



